7 Things Your Doula Wants You to Know
05 Aug 2018 Leave a Comment
in Most Popular
This Spring marked the 18th year that I have been serving families as a doula. In attending hundreds of births, I’ve learned a few things that are important to share with each client. Parents, if you are using a doula or are considering hiring a doula for your birth, here are some thoughts to keep in mind to make the most of this important doula/client relationship.
Keep me in the loop. A big part of the support that I am able to offer begins long before labor. I’m here to be your “walking birth wiki.” I’m way less scary than Dr. Google, and I love to talk about pregnancy and birthy stuff. Please, be in touch! Pick my brain. Ask me anything. I will offer information, share my resources, give you encouragement, and lend an empathetic ear to your concerns. I want to know if you go to the hospital for any reason, or have something happening that you are worried about. Keep me posted about what’s going on with your prenatal care. Even if it’s just a text that says “Hi, saw the doc, we’re all great!” I want to hear from you. It’s never “bothering me” to call. I’m going to let you set the pace for our communication; whether you text me once a day, email once a week, or call out loud once in pregnancy – that’s up to you. Everybody’s needs are different. I’m going to trust that you know that I’m available, and that you are in contact as often as you like. My commitment is to answer when you reach out, whether that’s once, or a dozen times.
Understand my role. You are the boss of this birth, and you have hired me as your doula. This means that I don’t tell you what to do. I can make sure we’ve discussed your options, and you tell me what’s right for you. As an experienced doula, I might have good relationships with your doctor, midwife, nurses, or hospital. Our being on a birth team together is something that will enhance your experience. Providing non-medical labor support is my role on the team. I will use the tools and skills I have to help you give birth the way you want to, while respecting the roles of medical professionals and the policies of the birthplace you have chosen. I am not there as a bodyguard or a bouncer. I don’t arrive prepared for combat. I cannot throw myself between a woman and the doctor who is responsible for her health and safety. If I tried that, the staff would throw me out and never let me or any other doula come back. I support your birth, and I also want to be able to show up for the next client who plans to deliver there. So, I don’t speak to anyone on your behalf. I don’t get to tell anyone what you will or won’t consent to. What I will do is remind you of your goals. I will encourage you to use your voice to ask questions that help you gather information, so that you have clarity to make your own decisions. I stand behind you in exercising your right to speak up for what you will accept or refuse.
Set yourself up for success. If you really want a natural waterbirth that’s “as close to a homebirth as possible,” the big teaching hospital with a 95% epidural rate and no tub is probably not the best place for you. Chances are pretty good that if you choose to give birth there, the birth you hope for isn’t going to happen. Make sure that your birthplace and your birth attendant are a good fit for what you have in mind. You, as the consumer, have a choice. Look into the facilities that are available to you. Ask what options they provide, and find out what they offer to support the kind of birth you want to have. The same is true for choosing your doctor or midwife. The practitioner who says “I don’t like doulas” isn’t very likely to be into the idea of other requests you make, either. Take personal responsibility for learning the rules of your attendant and your birthplace. Though I, as doula, may wish the best for you, my presence will not protect you from factors that come with the territory of the facility or practitioner you have chosen.
Prepare yourself for your birth. Take charge of readying yourself as fully as you can for birth in body, mind, and spirit. Participate in recommended childbirth classes, educate yourself about birth options and coping skills, and take excellent care of your body and your mental and emotional health. Seek out the support that you need to do this. Your power is already your own, and is not mine or anyone else’s to give to you or to take away from you. I do not empower your birth. I do not advocate for you. I support you in learning to empower and advocate for yourself. Likewise, I know a lot about having a baby, but I am not having your baby. I can make suggestions for positioning or comfort measures, and help you remember all of the ways that you have learned to cope with the intensity of labor. I can encourage you to ask for what you want. I cannot guarantee that your birth will be easy or uncomplicated. Labor is hard work, whether you have a doula or not. Birth is unpredictable, even when you’re well-prepared. When all is said and done, you are the one responsible for giving your consent and making your decisions. You are the one who will go through this process to become your child’s mother.
You have my unconditional support. My priority is to see that you know what your options are, and that you are making your own best choice. I want to understand your hopes and fears for this birth, so that you feel seen and heard. I will offer comfort measures in whatever way I can to help your experience happen in the way that you wish for. I will remind you of the priorities you have shared with me, and give encouraging words and hands-on support when you want it. I believe in you, and I know you can do this. I will not tell you that there is a right way or a wrong way to have your baby, and won’t leave your side if you change your mind about your plan. I will not judge you for the choices that you make. This is your body, your baby, and your birth. I trust you to make the best decisions for yourself. You have my support when you feel scared. You have my support when you think you can’t do it anymore. You have my support when you are crying. You have my support when you are angry, or irreverent, or unglued, or unlovely. You have my support in your joy. This is your birth. I’m here for you.
Our relationship will change. I love being your doula. I enjoy the whirlwind courtship of getting to know you well in a short time. I like hearing your stories about your life, the births of your other children, the story of how you met your spouse, the story of your own birth as your mother told it to you. I ask intimate questions that perhaps you hadn’t considered before, about your hopes, and how you cope with overwhelm, and what makes you feel safe. More than anything, I listen. Toward the end of your pregnancy, we may be talking once a week. In the last few days, we might be checking in every day. I might not ever know the names of your siblings, or where you grew up, or any of the other things your friends would usually know, but by the time your baby is born, we have forged a bond that is close and real. Then, after your baby is here and you are settled in as a new mother, I don’t see you much anymore, and we hardly ever talk. Please don’t take it personally. Know that I still care very much, even if I probably won’t make it to your child’s birthday party. Our relationship as doula and client happens for a finite period of time. I miss you. I love seeing pictures of your little ones as they grow. I cherish the memory of the time I have shared with you. Now I’m offering that same support to the next pregnant person. I’m just as occupied with her as I have been with you, and will be with you again if there is a next time. This is what doulas do.
I will always be grateful. Thank you for allowing me to serve as your doula. Thank you for inviting me into your life, your home, your birth space. Thank you for trusting me to support the birth of your beautiful child. Thank you for the honor and the privilege of caring for you through this part of your life. Every birth touches my heart. Every birth brings a lesson, and I am grateful for the learning that comes from your birth. I am grateful for this place where our paths crossed, and our life stories are woven together for this short while. Thank you always.
Like this article? Come “like” Jodi the Doula on Facebook here!
What Does a Doula Do?
29 Dec 2015 2 Comments
in Most Popular
Doulas are great, right? You’ve heard that a friend used one and loved her birth. Maybe your doctor or midwife suggested that having a doula would be good for you, too. Even the most reputable medical authorities (here’s looking at you, ACOG!) recommend birthing with a doula to decrease your chances of having a cesarean birth. But what exactly is a doula, and what do they do?
If you’ve been looking online for information about doulas, you’ve likely seen a hundred versions of something like this:
A doula is a woman trained in the physiology and psychology of birth, and in the art of providing labor support to birthing mothers during pregnancy, the birth process, and immediate postpartum period. It has been well-researched and documented that women who birth with doulas have shorter labors, are far less likely to have a cesarean birth, are less likely to use pain medication during labor, and report being much happier with their births. Women who have birthed with doulas are typically more likely to describe their birth in positive terms, and feel more attached to their babies.
Ok, good. People who birth with doulas are happier and are likely to have fewer medical interventions. That’s great news. Doulas are non-clinical professional labor support prople who work as a team with you and your doctor or midwife. Doulas provide a wide range of services to families of all sorts, in a variety of birth situations. But the question remains – what is it, exactly, that a doula will do for you? Provide support for birth, yes, but what does that support look like? Here are ten answers that you might not find in the standard “doula blurb.”
We get to know you. Before your birthing time ever arrives, and even before you choose to make the doula/client relationship official, we meet face-to-face. If you are inviting someone into a setting as intimate and vulnerable as your birth space, it’s important to first make sure that your doula feels like a good fit for you. (Not sure what questions to ask? Find some suggestions here.) I want to know how you function and express yourself in your daily life, when you aren’t in labor, because that will help me gauge the intensity of what you are experiencing when you are laboring and working hard. I want to know what you’ve heard about your own birth, about your partner’s thoughts on what his or her role will look like, and all about your hopes and preferences for your birth. We’ll talk about what we can do as a team to help your wishes happen.
We help you decide what to pack for the hospital. Have you seen some of the “what to bring” lists on the internet? Some are five pages long! (What exactly will you need a rolling pin, a blindfold and a deck of playing cards for?) Others are more like, “maybe bring a toothbrush, but the hospital might provide that, too.” We talk through all of the options that are available at your hospital or birth center. (Do you really need to bring your own pads and newborn diapers? Do you need to bring your own birth ball, or will your hospital provide one? Your doula knows the answer!) We’ll talk about what you might want to pack for yourself, your partner, and your baby, and what I might bring with me or be able to make out of what the hospital has on hand. (Think of your doula as your personal Birth MacGyver!)
We talk a lot about pain relief. Are you intending to have an unmedicated birth? Are you already certain that an epidural is right for you? Or are you somewhere in between, and want support in making the best decision for yourself when the time comes? The more I know about your preferences and priorities, the better I can support you in making them happen. I will recommend classes, books, and other educational resources that are a good fit for you. We can practice laboring positions and coping techniques together to help you prepare. I want to know which ideas really appeal to you, and which ones are not of interest to you at all. (Are you a guided meditation/self-hypnosis sort, or is dancing/moaning/swearing more your thing?) This helps me know what to suggest when you are in labor, and eliminates the need to try to have a discussion about it between contractions.
We help you know what to expect in labor. Long before you are ever in labor, we talk through what the day of your birth might look like, step-by-step. We discuss when to call your midwife, and when to call me. We’ll talk about things like what to do if you think your water broke, how to know when it’s really labor, and how to know when it’s time go without getting to the hospital too early or too late.
We listen. Doulas are professional non-judgmental listeners. I want to know what you are feeling, what you are thinking, and what you are going through. Whether you need to talk through something you are worried about, share your excitement, or vent to someone who will understand that you are feeling tired and done when you still have a couple of weeks to go, your doula is only ever a phone call away. Reach out as much or as little as you need to.
We answer the embarrassing questions. Did your mother-in-law tell you that eating too many spicy foods in pregnancy will make your baby rashy, and you want to know if it’s true? Want to know if eating your placenta is really a thing? That’s what I’m here for. Doulas are walking “birth wikis.” If I don’t know the answer, I know who will, and I won’t hesitate to say “call your doctor” when it’s appropriate to do so. Nothing is too embarrassing, random, weird, or icky. Really, asking me questions about sex in pregnancy or about your mucus plug is way less gross than Googling it, I promise. (But about that mucus plug – maybe just hold off on sending me pictures of it unless I ask.)
We provide continuous labor support. No matter which doctor or midwife is on call, or how many people are in labor in your hospital at the same time, or whether shift change happens for the nurse a time or two during your labor, you can count on your doula to provide one-on-one support from the time you are admitted to your hospital until the time your baby is born. We’ll suggest position changes and comfort measures. We’ll rearrange the furniture and break out all the tools it takes to help your labor progress. We’ll get you in and out of the shower or tub, and remind you to breathe. We hold the vomit bowl, and keep the cold washcloths coming. We know where the extra towels and blankets and chux pads are hiding. We keep your water bottle filled and remind you to hydrate. We tell you, as many times as you need to hear it, that you are strong. You can do this. All is well. We talk through your choices as they arise, and help you have confidence in your decisions.
Support is for partners, too. A good doula combined with a supportive partner makes for a real Dream Team in labor. A doula never replaces the role of a loving partner or family member. We encourage partners to be involved and included to the fullest extent possible. I’ll also make sure that he or she stays nourished and rested, so that he has the strength and energy to support you.
We help you feel safe. Birthing with a doula in a hospital is a lot like traveling to another country and bringing your own interpreter. As a doula, I’m fluent in the language of normal birth, and in the language of “hospital.” I help you know what’s normal and what’s not, and provide encouragement and reassurance when you need it. I’m protective of your privacy and modesty, if that’s important to you. I make sure the door to your room stays closed when someone enters or leaves. I am mindful of each little detail that makes you feel more comfortable in doing whatever you need to do to get your baby born. I pay attention to what’s going on around you that might not be said out loud, and gently bring things to your attention as needed. I facilitate conversations with your care provider, explain what’s going on and keep you focused if something unexpected comes up. I support you in the process of asking the right questions to get the information you want in order to make your own best choices. I provide a calm presence to sustain you and your support people through what might be a mentally, physically and emotionally intense experience.
We help you adjust to new parenthood. Doula support doesn’t end when the baby is on the outside. We’re also trained to provide support with infant feeding, newborn care, postpartum self-care and early parenting. Some doulas are even available to provide in-home postpartum care for several hours at a time in the early weeks. Your doula is part of your village. Nobody needs to feel like she is alone as a new mom. Reach out – support is exactly what doulas are there for.
Now that you know more about exactly what doulas do, you are ready to take the next step. You can email me at jodithedoula@gmail.com, or begin a search for a doula in your area by popping over to CAPPA’s website.
Best wishes, and happy birthing!
Doula Service and COVID-19
03 Dec 2020 Leave a Comment
in Most Popular
As of June 29, an Executive order from New Jersey Gov. Phil Murphy acknowledges the importance of doula support in maternal/fetal health, and specifies that doulas are not counted as additional support people, but are acknowledged as essential staff. This means that your doula may be by your side in labor in the hospital, along with your partner/chosen primary support person. So, the answer to “Can you come to the hospital for my birth?” is a great big YES!
We can talk more during an initial consult about the steps that are currently in place to keep everyone safe, and what to expect from doula services.
Birth services will continue to include three 1 1/2 hour visits prenatally to discuss birth options, comfort measures, and to create a personal birth comfort plan. These visits can be conducted by Zoom or Skype, or by phone, and can include virtual companionship to cover specific questions during medical provider office visits.
Conversation by phone is available after every medical provider office visit to discuss any questions or concerns you may have.
Unlimited phone call, text, and email support is available throughout pregnancy and the first 6 weeks postpartum.
Continuous labor support will be offered any time day or night.
Two 1 hour postpartum virtual visits will be available anytime in the 6 weeks following delivery, with continued unlimited phone, text, and email support to address any questions or concerns about infant feeding, baby care, or self care.
To best support the families and community in which we serve, your doula remains in communication with the New Jersey Department of Health and local hospitals and medical professionals to continue to provide the best possible support with consideration for current safety recommendations.
Availability for service is limited, so please call or text 856.419.3690 or email jodithedoula@gmail.com today to schedule your initial interview.
Talk soon!
Jodi
Doula Service and COVID-19
26 Mar 2020 Leave a Comment
in Most Popular
During this period of COVID -19 uncertainty, labor support is as important as ever. With safety recommendations changing day by day, limiting the support options available for birthing people, your doula remains at the ready to provide continuous informational and emotional support throughout pregnancy, birth, and the postpartum weeks. Currently, we are prepared to support the CDC’s recommendations surrounding COVID -19 by transitioning temporarily to virtual prenatal and postpartum appointments, labor support, and childbirth education.
As of March 17, 2020, there can be no visitors in local hospital waiting rooms during labor and delivery and only one (1) person in the delivery room. There can be no switch off between support people for the duration of the hospital stay. Only the client is allowed in the examination room during a visit at the prenatal clinic.
As of March 23rd, all home visiting services in New Jersey are to be offered as virtual services only.
In response to these state guidelines, while continuing to prioritize the support of pregnant and postpartum persons and in upholding the CAPPA Code of Ethics and Scope of Practice, labor doula services will be offered as follows:
Birth services will continue to include three 1 1/2 hour visits prenatally to discuss birth options, comfort measures, and to create a personal birth plan. These visits can be conducted by Zoom or Skype, or by phone, and can include virtual companionship to cover specific questions during medical provider office visits.
Conversation by phone is available after every medical provider office visit to discuss any questions or concerns you may have.
Unlimited phone call, text, and email support is available throughout pregnancy and the first 6 weeks postpartum.
Continuous labor support will be offered any time day or night by Zoom or Skype throughout labor and delivery and the first hour postpartum to ensure informed decision making.
Two 1 hour postpartum virtual visits will be available anytime in the 6 weeks following delivery, with continued unlimited phone, text, and email support to address any questions or concerns about infant feeding, baby care, or self care.
All current doula clients will remain in service with no interruption, and we are currently receiving new clients at this time.
To best support the families and community in which we serve, your doula remains in communication with the New Jersey Department of Health and local hospitals and medical professionals to continue to provide the best possible support with consideration for current safety recommendations.
Availability for service is limited, so please call 856.419.3690 or email jodithedoula@gmail.com today to schedule your initial interview.
Pregnancy and Loss: What NOT to Say
03 Oct 2016 Leave a Comment
in Most Popular
October is Pregnancy and Infant Loss Awareness Month. According to the Mayo Clinic, about 10 to 20 percent of known pregnancies end in miscarriage. The March of Dimes says that stillbirth affects one in 160 pregnancies. This means that you have most likely already known someone who has experienced pregnancy and loss, and perhaps you may again. If you haven’t, chances are, you will.
Doulas, nurses, midwives, doctors and other birth and medical professionals know well that pregnancies don’t always go as parents hope. We see the tiny footprints left on grieving parents hearts.
If someone you know has lost a pregnancy or experienced stillbirth, it may be difficult to know what to say or do to be of support. Don’t let discomfort stop you from reaching out. Acknowledging the pain of loss can help grieving parents cope. It’s OK to not know what to say, and even more important to know what not to say.
Here are ten “what not to say about infant loss” guidelines that birth and grief counseling professionals offer when someone you know has lost a baby.
“I know exactly how you feel.” You can’t possibly. No one can. Feelings are unique to the individual, and may change from moment to moment. Better to ask how she’s feeling, and be prepared that she may not have an answer for that.
“This is part of God’s plan,” “Everything happens for a reason,” or anything else that reflects your personal belief system. Though well intended, these may not be comforting things to hear. They may not fit at all with this family’s beliefs. They deny the emotions that are genuinely felt, and may even evoke anger. Best to keep your beliefs to yourself, and find your own comfort in them.
“Look at what you have to be thankful for.” Chances are they know this already. Yes, they’re alive, and a couple still has each other, or may already have other children, or another chance. The time will come to think about these things. Right now, that’s not what’s important.
“You should…” or “You will…” Nobody needs unsolicited advice or to be told what to do. If you have information to share, and you are sure it is welcome and asked for, it is best to begin it with “One option is…”, or “You might consider…”, with no pressure or expectation.
“Tell me if there’s anything I can do.” Keep in mind that a person in grief may not have the energy or motivation to even know how to ask, or what to ask for. They might feel guilty or uncomfortable for being on the receiving end of so much attention. It’s better to be willing to take the initiative. “I’m stopping by the store on the way to your house. What do you need?” may be an easier question to answer. Drop off food, throw in a load of laundry, or do the dishes that are in the sink without being asked. Keep visits short, unless you have been asked to come and stay a while.
“You look great.” Appearances can be deceiving, and it’s important for grieving people to know that there’s no pressure to hide feelings through keeping up appearances. Know that life to them may not ever feel the same. The pain may lessen over time, and life does go on, but the sadness may not ever completely fade away.
“I’m having such a hard time because I feel so sad for you!” If you are having difficult feelings about someone’s loss, seek out your own support people who are not in the inner circle of the grieving family. It is not the grieving parent’s responsibility to listen or offer comfort. They are deeper in the pain of their loss than anyone else could be. Many grieving parents express that people who call or visit, while intending to share their loving concern, are really looking for the parents to reassure them that everything is ok, when it isn’t.
“Grieving for this long can’t be good for you. Shouldn’t you feel better by now?” Grief doesn’t have to happen in normal, predictable, measurable stages. It can be messy, with highs and lows, forward motion and setbacks. Everyone experiences this differently. Just as there is no set timetable for birth, there is no set timetable for healing. Recovery from grief may take weeks, months, or years. There will be plenty of people who convey the message to grieving parents that they have been grieving for too long. Please, don’t be one of them.
“I don’t want to say the baby’s name and upset them!” If someone has lost a baby, whether early in pregnancy or at full term, don’t be afraid to talk about the baby by name, if a name has been chosen and shared with you. This name is etched forever in a parent’s heart, and hearing it will provide comfort and assurance that the child is real and will not be forgotten.
It’s OK to talk about infant loss. Break the silence. Without forcing a grieving person to open up, let her know that she has permission to talk about her loss if she wants to. We can begin by simply asking, “Do you feel like talking?” Follow her lead when she’s ready, listen with compassion, and let her know that you are there. That’s enough.

It All Started with THIS
27 Aug 2016 Leave a Comment
in Most Popular
I’ve had a whole five days now of THIS:
And it all started with THIS:
An empty coffee cup on a Monday morning is a terrible thing. So, I walked off in search of THIS:
In my own kitchen, in the house where I live, where I have walked at least a thousand times, my toe collided with THIS:
THE STEPSTOOL. Which has lived without incident on the floor in the kitchen for as long as it has been our kitchen. The thing I’ve stepped up on every time I’ve needed to reach into the upper cabinets, because SHORT PEOPLE PROBLEMS, Y’ALL.
And because two solid pbjects that have both have weight and mass cannot occupy the same space at the same time (and I told my ninth grade science teacher I’d never need to know this stuff!) my toe did THIS:
Nope, not gonna show it. Some things just have to be imagined. Ew, and then unimagined. Just think of puppies, envision the calm blue ocean… it’ll be ok.
So, I went to the emergency room, right? WRONG.
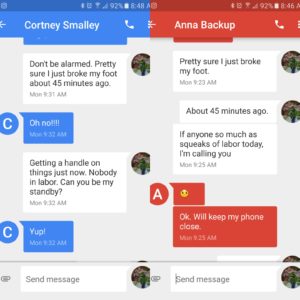
Eventually, yes. But first, I did THIS:
Texted my backups. Both of them. Because WHAT IF SOMEONE GOES INTO LABOR RIGHT NOW? Break a bone, break a water bag. I’m pretty sure that’s a real saying that I maybe just made up right now. But when you’re a doula, that’s what happens. Ninth grade science teacher didn’t cover why that’s true, but I believe a certain Mr. Murphy may have.
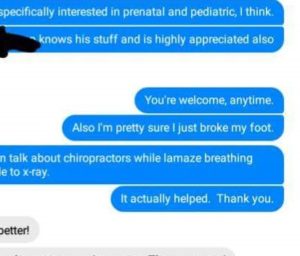
Waiting for the Uber to take me to ER, took care of THIS:
Because what else would a doula do besides focusing on a distraction (like answering a question about which chiropractors I love) while lamaze breathing and texting a neighbor for a ride to the emergency room?
So, now my view is a whole lot of THIS:
And I can’t wait for this fat purple foot to fit back into THESE:
I’m bored. I’m a little frustrated. I’ve watched a lot of TV and done a lot of phone time this week, rescheduling classes and clients. I’d like to get up and drive or throw in my laundry or even THIS:
Hi, vacuum cleaner! Miss me?
But if a baby should need to arrive today, I’m not worried. I’m grateful for a strong team of professional and reliable colleagues. If someone went into labor, I knew that my clients would be in excellent hands as I rest and continued to heal. A good doula knows to prepare for the unexpected. “What if you were suddenly unavailable” and “Who is your backup?” are important questions to ask your doula, and even more important for your doula to have a solid answer for!
Because life can happen, just like this!
How Many Doulas Does It Take to Change a Lightbulb?
01 Aug 2016 Leave a Comment
in Most Popular
One, but only if it’s her own lightbulb. Otherwise, I’m not the homeowner or the electrician, so it isn’t my call. However, I am familiar with the process, and would be happy to talk you through.
First, do we know that the light bulb must be changed right now? Are there more urgent matters at hand, like fire or glass on the floor? Is everyone safe? Do we have time to talk this through? OK, good.
The benefit of changing the light bulb would of course be having more light in the room. Is that your preference? Great.
The risk of changing the light bulb would be falling off of a ladder, but that’s relatively low in this case because the lamp is on the table and the likelihood of your needing a step ladder is minimal.
Of course, it’s another option to use a camping lantern, or light a candle or use a string of twinkling Christmas lights as long as that’s appropriate and safe for the space it’s in. What ideas might you have about that?
Or, you could choose to do nothing right now. It’s still daylight out, and the lamp is decorative, and perhaps you aren’t planning to keep it. I remember you’ve said that Aunt Mildred meant well when she gave it to you, but it really isn’t your style. It’s entirely up to you.
If you are worried even a little, call your contractor or an electrician. They may assure you that this isn’t an emergency, or they might want to talk with you in person to let you know of ways that they can help you make a plan for this. They might recommend installing overhead canister lighting fixtures, but I’m really not the person to ask about that.
What matters most is that you are making the decision in this that is right for you. I want you to be content with your lighting choices. Let me know how I might be of support.
There’s no pressure to make a rushed decision, take some time, mull that over, talk to your partner, and let me know what you think. And if you change your mind about it later? That’s ok too. It’s your lightbulb. You can do that.
When “Rare” Becomes Real
15 Apr 2016 2 Comments
in Most Popular
If you’ve been following recent news at all, you’ve no doubt heard the hubbub about the new documentary Vaxxed, which was pulled this week from the Tribeca film festival in New York, where the film was scheduled to be shown. Robert DeNiro is under fire in recent media, both for pulling the film from the festival and for stirring up the ongoing controversy around vaccine safety. Vaccine controversy is hardly anything new – it’s a question that parents have been facing for the last twenty years.
As a doula, I hear “the vaccine question” from many families I work with. My answer is always, quite simply, “It’s not ever my role to give medical advice. This is, however, an important topic to learn about and have an informed conversation with your child’s doctor about the right decision for your own family.” I will gladly recommend evidence-based resources to support parents in educating themselves. Professionally, I’m Switzerland – as neutral as can be. I typically don’t even mention my own point of view, because it’s irrelevant to the decision another family may make.
A quick Google search would have us believe that there are only two extreme schools of thought. One side of the fence says “All vaccines are bad, the general public is brainwashed” and the other states just as clearly that “all scheduled vaccines are necessary, and only the misinformed Tin Foil Hat Brigade thinks otherwise” There is, however, an often-unmentioned middle ground. This is one parent’s story of what living in the invisible no-man’s-land really looks like.
Eighteen years ago, when my son was three months old, at his standard well-baby checkup he received three shots. Having been through the usual routine with my older child, this was nothing new. What happened in the aftermath, however, became a completely different story. My son had what is generally referred to as an atypical reaction. It’s nothing unusual for babies to run a slight fever and be a little cranky the day after shots. In the wee hours of the night, a few days later, however, my baby wasn’t just fussy, he screamed. I don’t mean he cried very hard – this was a high-pitched, piercing wail that lasted for hours, unending. He ran a high fever. The soft spot on his head began to bulge. The membrane that surrounds his brain was swelling. This is called encephalopathy.
The Center for Disease Control, the same CDC that advocates for routine scheduled vaccination, notes that this encephalopathy is a real, though rare, known possible side effect of one of the three vaccines he had received. Our doctor provided excellent medical care, and access to solid information. The US government has a Vaccine Adverse Event Reporting System in existence since 1990, and a VAERS report was filed about my child.
I am acutely aware that this is unusual, though the exact statistics of specifically how uncommon are harder to pin down. The Center for Disease Control (CDC) states that “approximately 30,000 VAERS reports are filed each year. About 85-90% of the reports describe mild side effects such as fever, arm soreness, and crying or mild irritability. The remaining reports are classified as serious, which means that the adverse event resulted in permanent disability, hospitalization, life-threatening illness, or death.” The probability of serious adverse effects is minimal, with only 3000-4500 serious adverse effect reports per year, out of the over ten million vaccines adminstered per year to infants under the age of 12 mos. This statistic can be reassuring to some parents. However, when your own child becomes the statistic, the viewpoint changes.
The challenges we have faced were only beginning. My baby stopped smiling and cooing. His milestones, like rolling, crawling, and walking were delayed. Other developmental delays began to follow. Speech delays caused him to be only minimally verbal until the age of six. He didn’t develop a dominant hand (become left- or right-handed) until seven. He was in physical and occupational therapy until the age of eight. A visual disability thrown into the mix meant that learning to read at all was delayed until the age of nine. Writing with a pencil (illegibly, but intentionally) wasn’t obtained as a skill until age 11. He didn’t sleep through the night until he was 12 – years, not months – when it was finally accurately diagnosed that an existing neurotransmitter deficiency requires medications that tell his body when to wake up and when to fall asleep. He has moderate multiple sensory processing challenges, and an autism spectrum diagnosis. It has taken many qualified and dedicated professionals to figure out how my kid learns, working as a team to ensure his success. He was homeschooled or tutored at home until fifth grade, when he was mainstreamed into school with a 504 (a document that provides exceptions for children with disabilities) and an Individual Education Plan (IEP.) This is the reality of living with a special needs child.
So, do I believe that vaccines cause autism? Put simply, no. Current evidence bears proof that most reactions, if they happen at all, are mild, and the benefits outweigh the risks. Most children who receive them will be fine. My child, however, will not receive another one. With no explanation for why the extreme reaction happened, it’s not worth the risk to his health and safety. I’m grateful for herd immunity that occurs when most children are vaccinated against disease, because that’s what keeps my child safe from these diseases.
On a positive note – he’s come a long way. In a month, he’ll be graduating high school with honors and will attend college on an engineering scholarship. He’s in the National Honor Society, plays on the football team, loves to act and sing, and has a fondness for really corny jokes. Social skills have had to be vigilantly taught in baby steps, and he’ll never be neurotypical, but he’s going to be ok. He’s a little awkward, perhaps, but given that he’s going to be an engineer, it’s possible nobody will find that strange.
I don’t blame “modern medicine.” I like aromatherapy and all, but if my kid has appendicitis, we’re going to the hospital. I’m aware that the highly-publicized “MMR Causes Autism!” Andrew Wakefield study from 1998 has been debunked. I don’t think our pediatrician was participating in any sort of conspiracy or “cover up” when he recommended vaccinating our baby. While I do also believe that diet and lifestyle are important factors in everyone’s health, I work within the health system. I’ve witnessed lives being saved by modern medicine with my own eyes. I run an evidence-based doula practice, and I believe in science. My son has been seen by numerous specialists, including heads of department in a reputable children’s hospital.
All of that said, the missing piece here becomes glaringly obvious. We still don’t know why this happened, and we are not alone. Parents across the country, another 3000-4500 serious VAERS reports per year, are telling their stories of similar events. Their babies were fine, got vaccines, and weren’t fine anymore. Some have serious illness, and some are no longer living. With 23.2 million children under the age of five living in the US at the time of my son’s birth, even being one in 10,000 is no longer a small number, and it’s only growing larger.
Most children will be fine. A small percentage will have reactions that are classified as severe. That small percentage happens to a few thousand children a year. Unfortunately, none are born with stickers on their foreheads that say, “I’m the one who’s going to be injured,” but there is hope that perhaps there are other clear signs that we can learn to see. This is worth attention. We need to learn more.
There are many theories currently being suggested by respected medical authorities. Is there a genetic component that makes some children more vulnerable to adverse events than others? Maybe. I have multiple autoimmune diagnoses, and my son’s father had severe mental health issues. In fact, at the age of 40, my son’s father had an adverse reaction to a routine Hepatitis B vaccine, developed a lesion on the cerebellum of his brain, and was hospitalized for a week.
Were environmental factors involved? Maybe. We do live in New Jersey, where the autism rates in the US are at their highest, along with our air and water pollution levels. Or, on the other hand, perhaps our early autism screening system just works more effectively in New Jersey than it does elsewhere. The thing is – we don’t know. Science can’t tell us yet how to discern who will be fine, and who is more likely to not be fine. “Why did this happen?” is a question that my family, and many others like mine, still have unanswered.
This is where research is leaving a gaping hole. Studies are being conducted left and right to prove that vaccines don’t cause autism. What isn’t being focused on, however, is the answer to WHY, exactly, these serious reactions happen to some children and not others, and what we can do to make it safer for everyone.
What’s being brought to light, here, is that research needs to be done on the “maybes,” so that they become answered. When we know more about the facts, when we learn the “why,” we can make a more effective plan than “It probably won’t happen to you.” This happens. It’s rare, but real. I’m not angry, but I am aware. The parents who live with this reality are simply asking for answers. All we’re looking for is the truth. No tinfoil hat required.
Jingle Balls
20 Dec 2015 1 Comment
in Most Popular
When I never know what tomorrow may bring, getting holiday baking done can require some juggling. Jingle Balls to the rescue! These are super easy, and can be done in short bursts of activity. They store well in the fridge throughout the holiday season, and are always a hit.
I’ve been asked for the recipe, and i have to confess that there really isn’t one. It’s too simple to be called a recipe. There used to be one, somewhere, and it was called something else entirely, and I’ve changed it to suit myself.
Here’s how it’s done.
Step one: Bake one boxed cake mix, any flavor. I like chocolate.
Step two: As soon as the cake is out of the oven and still very hot, scrape it into a big mizing bowl, dump a tub of frosting in it (chocolate again,) and stir it all into moosh.
Step three: Put it in the fridge until you have time to deal with it – could be a couple of days. Snitching occasional fingerfulls of the lovely moosh straight out of the bowl is suggested.
Step four: Roll moosh into walnut sized balls, put them on a cookie sheet, put them in the fridge.
Step five: Promptly ignore them until the moment you say “Oh, geez, I have people coming over, and I could get called to a birth tonight, I’d better get these done.”
Step six: Melt a bag of chocolate chips (I do about a third of the bag at a time, and use a cereal bowl in a saucepan as double burner, because who has room for a double burner in her cabinets anymore?) Throw in four or five balls at a time, swish them around until they’re covered in melted chocolate chips (Oh, I also throw in about a tablespoon of coconut oil, just to mnake the glaze a bit thinner), use two forks to lift them out, and put them back on the cookie sheet.
Step seven: Chill until the chocolate is firm, and ta-dah! Jingle Balls!
There you have it! A totally simple and impressive holiday treat, compatible with busy lives and procrastination! Enjoy, and Happy Merry from Jodi the Doula to you!
What Should I Buy for the Baby?
05 Oct 2015 2 Comments
in Most Popular
At prenatal visits, I’m often asked what the necessities are for bringing baby home. The lists offered by most baby registries are long and overwhelming. Keep in mind, too, that the more “stuff” you register for, the more profit the store makes when your friends and family come to shop for you there. What’s a new family to do?
In short, as long as you have your breasts, your arms, and some diapers, you’re going to be ok in the beginning. Tiny babies don’t need much. Here are a few things that, as a doula, I see most families use and enjoy.
1) A Carseat. Don’t skimp here. Get the best one you can afford, and please make sure that it’s correctly installed. Call your hospital and ask if they offer carseat safety checks, or if they know who does. According to the National Highway Traffic Safety Administration, although most parents believe that theirs is installed correctly, seven out of ten carseats are improperly installed. Get it checked by a professional. I’m serious about this part.
2) Onesies, newborn gowns, and sleep sacks. Tiny babies tend to be leaky at one end or another several times each day, and require changing of diapers and clothing. It’s amazing how much laundry one little person can generate in the course of a week! Onesies are easy because they’re simple, soft, and low-fuss. If a diaper is a real blowout, the folds on the shoulders of a onesie allow the whole thing to be pulled straight down toward the baby’s feet – no need to take a messy thing off by pulling it over baby’s head. Newborn gowns, which have long sleeves and simple elastic at the bottom, are the best invention ever when, at 3am, you can’t keep your eyes open when your little one needs a diaper change. They pull up and pull down – easy to do one-handed, and no tiny snaps to fuss with in the dark. Sleep sacks are a warmer version of nightgowns, for when the temps are cooler. Remember that your babe will only be in newborn sizes for about five minutes, so don’t buy a ton. Half a dozen onesies and gowns, and a sleep sack or two is a good place to start.
3) Light, thin blankets. These are great for covering baby and parent for skin-to-skin time, which is so important for bonding and breastfeeding success in the early days. They’re also great for throwing over Aunt Irene’s shoulder when she asks to hold the little one who has just been fed, so that she doesn’t get blurped on. If swaddling is your baby’s thing, light blankets are just the right weight. Remember that babies don’t need blankets for sleeping, though. That’s what nightgowns and sleep sacks are for.
4) A safe place to sleep. In the “Safe Sleep Seven” handouts written by Sweet Sleep author Dianne Wiessinger and published by La Leche League International, guidelines are given for the safety of babies who cosleep with parents. The American Academy of Pediatrics, in their guidelines for safe sleep, recommend room sharing, though not necessarily bed sharing, in the early weeks. Whether bed-sharing or room-sharing, newborns need to be close to their parents, and aren’t ready for cribs in separate rooms just yet.
5) A sling or soft carrier. Very small babies tend to be happiest when they are in-arms and at-breast. How is a parent to get anything done that requires two hands? Babywearing is a great solution to keep parents and babies both happy. There are many soft carrier options to choose from. Babywearing International has good safety guidelines on their site, along with great information on how to choose the carrier that’s right for you.
6) One safe place to set baby down. There are so many options – bouncy seats, swings, rocking seats, and the list goes on and on. Really, it’s not necessary to have one of each. No need for your house to look like you’ve decorated in Early Fisher Price. Just one thing will do. Pick one. Will your baby like it? Probably not, at least in the beginning, but in a few weeks, the beloved bouncy seat may be the one thing that allows you to get a shower.
7) A way to get baby fed. If you are planning to breastfeed, hold off just yet on the bottles, pacifiers, sterilizers, and warmers. Breastfeeding has a bit of a learning curve in the first month. It’s best to get really good at breastfeeding before adding other things into the mix. That can come later.
8) Diapers and wipes. Whether disposable or cloth, you’re going to use a lot more of these than you might think you will.
9) SUPPORT. Whether you have a postpartum doula or family and friends who can pitch in, let someone else do the laundry, the errands, the cooking and the housework. It’s Mom’s job to take care of the baby, and it’s everyone else’s job to take care of Mom.
That’s it – the “Doula’s List” of what you really need. What would you add? What did you use more than you thought you would? What did you have that didn’t get used at all? Leave your thoughts in the comments below.